Our Work
Our Work before & after



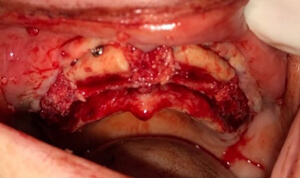

Ridge Augmentation Using Bone Blocks in an Atrophic Maxilla for Future Implant Placement
Patient Background
The patient was a female who wore a removable upper denture. She presented an atrophic maxilla with significant bone loss in the upper jaw, limiting the available bone volume for conventional dental implant placement.
Chief Complaint and Treatment Goals
The patient expressed dissatisfaction with her removable upper denture, citing concerns about stability, function, and comfort. Her primary goal was to transition to a fixed dental prosthesis to improve oral function, enhance esthetics, and increase overall satisfaction with her dental restoration.
Clinical Assessment
Clinical and radiographic examinations confirmed the presence of a severely resorbed (atrophic) maxilla with insufficient bone height and width to support dental implants without additional surgical intervention. The patient was otherwise healthy and motivated for advanced implant therapy.
Treatment Plan
- Ridge Augmentation: ridge augmentation was planned to address the inadequate bone volume. This procedure aimed to rebuild the alveolar ridge, providing a stable foundation for future implant placement.
- Bilateral Sinus Lift: bilateral sinus lift procedures were indicated due to the proximity of the maxillary sinuses and the insufficient vertical bone height in the posterior maxilla.
- Implant Placement: dental implants would be placed strategically in the maxilla to support a fixed prosthesis after adequate healing of the augmented sites.
As part of the ridge augmentation, the use of allogeneic bone blocks was planned to reconstruct the severely atrophic maxillary ridge. Allogeneic bone blocks offered a reliable solution for augmenting bone volume and contour, especially in complex cases with significant horizontal and vertical deficiencies. Their structural integrity allowed for precise adaptation to the recipient site, promoting stable integration and support for subsequent implant placement. An additional benefit of this approach was the restoration of the alveolar ridge profile, which contributed to the gain of lip support. Improved lip support enhanced facial esthetics and provided a more natural appearance, addressing both the functional and cosmetic expectations of the patient.
Expected Outcomes
This comprehensive approach aimed to provide the patient with improved oral function, enhanced esthetics, and greater comfort compared to her current removable denture. By addressing the atrophic maxilla with ridge augmentation and bilateral sinus lift, the foundation for successful, long-term implant rehabilitation was established.




Gum Recession Treatment with CTG Procedures
Chief Complaint:
A female patient presented with concerns about gum recession in her upper teeth. She reported increased tooth sensitivity, especially to cold, and expressed esthetic concerns due to the visible exposure of tooth roots when smiling. She was particularly distressed by the appearance of her anterior maxillary teeth and was motivated to seek a long-term solution.
Treatment Goals:
The patient's primary goals were to:
- Achieve root coverage in the affected areas.
- Improve esthetic appearance of her smile.
- Reduce or eliminate dentin hypersensitivity.
- Enhance periodontal health and stability in the long term.
Clinical Assessment:
Upon examination, the patient exhibited localized recession defects in the maxillary arch, most notably in the canine and premolar regions. The gingival margins were apical to the cementoenamel junction (CEJ), with mild loss of attachment but no active inflammation. Probing depths were within normal limits, and plaque control was acceptable.
Treatment Plan:
The treatment plan included a Connective Tissue Graft (CTG) procedure to address the gingival recession. The approach involved:
- Harvesting a subepithelial connective tissue graft from the palatal donor site
- Creating a recipient site via partial thickness flap in the areas with recession
- Placing and securing the graft to promote root coverage and tissue thickening
- Providing post-operative instructions and close follow-up to monitor healing
Outcome Goals:
The intended outcomes of the CTG procedure were to:
- Achieve partial to complete root coverage, particularly in the esthetic zone.
- Increase the thickness and width of keratinized tissue.
- Provide a more harmonious gingival contour.
- Reduce sensitivity and improve overall patient comfort and satisfaction.
The patient reported being very satisfied with the results of the procedure. She noted a significant reduction in sensitivity, especially when consuming cold foods and beverages. She was also pleased with the improved appearance of her gums, describing her smile as "more natural and healthy-looking."






Gum Recession Treatment with FGG Procedures
Chief Complaint
A male patient presented with concerns about receding gums in the lower jaw. He reported increasing sensitivity to cold, as well as discomfort during toothbrushing. His primary concern, however, was the progression of gum recession over time, and he expressed a desire to prevent further deterioration of his gum tissue.
Treatment Goals:
The patient's main goals for treatment were to:
- Stabilize the gingival margin to prevent further recession.
- Increase the zone of keratinized tissue.
- Improve oral hygiene access and reduce discomfort during brushing.
- Reduce sensitivity associated with exposed root surfaces.
- Enhance long-term periodontal health.
Clinical Assessment:
Clinical examination revealed generalized gingival recession in the mandibular teeth. The affected sites had:
- Minimal to no attached gingiva
- A thin periodontal biotype
- No signs of active inflammation or deep periodontal pockets
- Exposed root surfaces, contributing to hypersensitivity.
The recession was exacerbated by anatomical factors, such as thin tissue phenotype, and mechanical trauma from brushing.
Radiographic assessment confirmed there was no significant alveolar bone loss, and the teeth exhibited normal periodontal support.
Treatment Plan:
The patient was scheduled for a Free Gingival Graft (FGG) procedure aimed at increasing the width of keratinized gingiva and stabilizing the gingival margin. The surgical plan included:
- Harvesting a thin epithelialized graft from the palatal donor site
- Preparing a recipient bed apical to the area of recession
- Suturing the graft into place to promote tissue integration and healing
Outcome Goals:
The goals of the FGG procedure were to:
- Increase the width of keratinized tissue in the mandibular anterior region.
- Provide a stable band of attached gingiva to resist future recession.
- Facilitate plaque control and reduce brushing discomfort.
- Minimize hypersensitivity associated with root exposure.
- Support long-term periodontal stability and maintenance.
The patient reported a positive experience and high satisfaction with the outcome of the procedure. He noted that the post-operative discomfort was minimal and manageable with the prescribed medication and care instructions. Within a few weeks, he observed a noticeable increase in gum thickness and felt more confident during brushing due to the reduced sensitivity and improved tissue resilience.



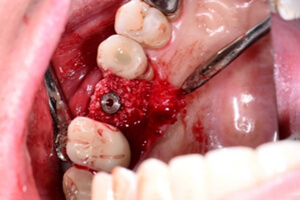
Case Description: GBR with Biologics for Peri-Implantitis at Implant #14
Chief Complaint:
A male patient presented with concerns about progressive bone loss around implant #14. He reported discomfort in the area and was worried about the implant's long-term prognosis due to peri-implant inflammation.
Clinical Assessment:
Clinical examination revealed increased probing depths (7 mm) with bleeding on probing and suppuration around implant #14. Radiographs showed significant vertical bone loss adjacent to the implant. The implant remained stable with no mobility detected. The diagnosis of peri-implantitis was confirmed.
Treatment Goals:
- Eliminate peri-implant infection.
- Regenerate lost peri-implant bone tissue.
- Restore soft tissue health around the implant.
- Preserve implant stability and function.
Treatment Plan:
The patient underwent a surgical procedure involving Guided Bone Regeneration (GBR) combined with biologics to enhance healing and bone regeneration. The steps included:
- Full-thickness flap reflection for access and decontamination of the implant surface
- Mechanical and chemical cleaning of the implant threads
- Application of biologic agents (platelet-rich plasma) to promote osteogenesis and soft tissue healing
- Placement of bone graft material and a resorbable membrane for guided bone regeneration
Postoperative instructions included antibiotic therapy, antiseptic mouth rinses, and regular follow-up visits.
Outcome Goals:
- Reduction of probing depths to ≤4 mm
- Resolution of bleeding and inflammation
- Radiographic evidence of bone regeneration around implant #14
- Patient comfort and satisfaction with the functional outcome
Results:
The patient demonstrated favorable healing without complications. At the 6-month follow-up, clinical measurements showed reduced probing depths and absence of bleeding on probing. Radiographs confirmed successful bone fill in the defect area. The implant remained stable and fully functional.
Patient Feedback:
The patient expressed satisfaction with the treatment outcome. He reported relief from discomfort and appreciated the improved stability and health of the implant site.



